Lors d’une entorse, il est toujours préférable de consulter le médecin traitant et de bien suivre le traitement, notamment la rééducation éventuellement prescrite auprès d’un kinésithérapeute. L’entorse entraîne en effet une perte importante de la force musculaire au niveau de l’articulation atteinte En cas d’entorse de cheville, talons hauts et terrains accidentés seront le plus souvent à éviter.
Your health
-

Live better in movement
-

Live better with your desire for a child
-

Live better with your osteoarthritis
-

Live better with your skin
WHAT IS TRAUMA?

Sprains and tendinitis in the front line!
Joints are highly sought in daily life and usually put under strain when practicing some sports. Joints may be subject to traumas that may be violent (knocks, shocks), or insidious but repetitive to end up with sprains and tendinitis.
These pathologies constitute the most frequent reasons for consult in common trauma with approximately 6 million consults per year for tendinitis and not less than 6000 consults a day for one ankle sprain (1)!
Sprains and tendinitis are trivial but painful and disabling and must not be neglected. They may cause complications and must be treated appropriately.
What is the difference between a sprain and tendinitis?
- A sprain is a damage to one or more ligaments in a joint, leading to painful inflammation with eventual swelling (oedema). Ligaments are fibrous structures that maintain the joint by connecting bones resting on both sides. These ligaments are poorly expandable and any forced movement, excessive traction leads to extreme stretching, even a rupture. That is a sprain.
- Tendinitis, on the other hand, corresponds to damage to the tendon. The tendon connects the bone from a joint to a muscle same as a rope. Its passes on the muscle strength and allows the movement of the joint. A too intense or repetitive effort induces an irritation and inflammation of the tendon. Unlike the sprain which is usually acute, tendinitis is generally progressive. The movement becomes difficult and painful, it’s tendinitis.
REFERENCE
1) Leuret A. et al. L’entorse de cheville au service d’urgence. Conférence de consensus en médecine d’urgence – SFMU Actualisation 2004
Les entorses
Lésions traumatiques les plus souvent rencontrées (2)
Les entorses de cheville, suivies des entorses du poignet et du genou sont les lésions traumatiques les plus fréquentes.

Figure 1: Source IMS Santé – Etude EPPM – S90-S99 / S60-S69 / S80-S89 / S40-S49 / S50-S59 / S70-S79 / T00-T07 – Automne 2014 – nombre de diagnostiques
Les signes
L’entorse se manifeste par une douleur assez variable, son intensité n’est pas toujours proportionnelle à la gravité. Le plus souvent, un gonflement (œdème) apparaît plus ou moins rapidement au niveau de l’articulation ainsi qu’un hématome, témoins d’une réaction inflammatoire aiguë, importante, au niveau des ligaments.
Qui ?
Du simple faux pas à l’accident de sport, tout le monde peut se faire une entorse. Il existe cependant des personnes prédisposées et des situations à risque.
- Personnes âgées ou sportives
- Antécédents d’entorses
- Faiblesse musculaire, manque d’exercice
- Surpoids
- Chaussures inappropriées
- Terrain accidenté
L’articulation la plus sujette aux entorses est celle de la cheville et 15 à 20% de celles-ci proviennent d’un traumatisme sportif. Viennent ensuite les entorses des genoux et des doigts.
Les soins
Quelle que soit la gravité de l’entorse, les premiers soins restent les mêmes.
Les 1ers gestes
Afin de limiter les complications, il est recommandé d’adopter au plus vite ce que l’on appelle le « protocole GREC » (pour Glace, Repos, Compression, Elévation) (1) :
- Glace: appliquer de la glace (poche remplie de glace, “bombe de froid”) tout de suite puis 4 fois/jour pour réduire la douleur et le gonflement
- Repos : limiter l’activité, s’aider de cannes anglaises s’il s’agit du genou ou de la cheville
- Elévation : maintenir le plus souvent possible la zone atteinte surélevée pendant la journée et la nuit (coussin sous le matelas …)
- Compression légère, seulement pour les personnes averties : immobiliser l’articulation par un bandage ou une attelle souple
REFERENCES
1 – Leuret A. et al. L’entorse de cheville au service d’urgence. Conférence de consensus en médecine d’urgence – SFMU Actualisation 2004
Faq
Tendinitis
Frequency of localization of Tendinitis
Many parts of the human body may be affected, first of all, the shoulder, elbow (“tennis elbow”), the knee but also the ankle, the hip, the wrist…
Figure 2 : Source IMS Health – EPPM Study – M75.0 / M75.1 / M75.3 / M76.5 / M76.6 / M76.8 / M77.1 – Fall 2014 – number of diagnosed
Signs

The main symptom is pain at affected tendons. Depending on the significance of the lesion, pain may be perceived as a simple discomfort when moving or a constant shooting pain preventing any movement of the affected joint.
Tendinitis is favoured by age, overweight, presence of pre-existing static disorders but also by inadequate working conditions (repetitive heavy load carrying, inadequate technical gestures), excessive sport practice (excessive use of joints)(1).
When to consult?
Tendinitis is not a matter of urgency, however it may rapidly become disabling to the personal and professional life.
Therefore, do not hesitate to consult when:
-
- Pain is persistent and lasts for 2-6 weeks in spite of adequate treatments
- In case of a tendinitis due to a professional activity: An interview with the occupational doctor is necessary
- Movement become impossible: There must be a ligament rupture
REFERENCES
1- Bard H. Tendinopathies : étiopathogénie, diagnostic et traitement. EMC Appareil Locomoteur 2012;[15-146-A-10].
First acts in case of pain
- Stop the activity to put your joint at rest
- Apply cold: Ice pack, “cold spray”
- Wear light compression stocking if possible to limit tendon elongation during movement: Elastic bandage, kneepad…
- Take topical analgesics and/or topical anti-inflammatory medicines as the inflammatory component is major.
Medical care
Upon examination, the doctor will try to locate the affected tendon and assess the impact of tendinitis on activities. In some cases, additional imaging tests may be necessary(1). He/she will then prescribe medicinal treatments and/or adequate functional treatments (1).
REFERENCE
1 – Agence Française de lutte contre le dopage. Guide agréé par le comité médical consultatif pour les AUT sur le fondement des travaux du Dr RODINEAU
Faq
PROCREATION: A COMPLEX PROCESS
What is more essential for a couple than to have a child? Sometimes, an unfulfilled desire…
Fertility varies from one to another and depends on sexual activity: The probability of pregnancy during a menstrual cycle is low, in the range of 20-25% (1). Fertilization, as a prelude to pregnancy, is in fact a complex physiological process that is regulated by multiple factors, including hormonal ones.
REFERENCE
(1) – BEH, INVS, N°7-8-9 du 21 février 2012
Fertility
Fertalization in short
Fertilization is the outcome of the encounter between an ovum and a sperm cell, two reproductive human cells. The most favourable moment to this encounter is before the 13th day of a 28-day cycle, which means at ovulation.
Ovulation: The ovum (egg) develops in the ovary inside the “follicle” then released toward the fallopian tube. This process is carried out under the control of brain hormones (FSH and LH); which are themselves influenced by hormones that are secreted by ovaries.
The “encounter”: It happens within the tube, where sperm cells swim up after their release in the vagina. Sperm cells must be in a sufficient large number, mobile and find a favourable milieu in the cervix, notably the mucus; which quality depends on cerebral and ovarian hormones (estrogens and hCG).
Fertilization itself: Only one of these sperm cells will fertilize the egg. An egg-cell is therefore created, it predetermines the embryo. This cell starts dividing and begins its descents towards the vagina.
Implantation: The future embryo reaches the uterus. It implants within the endometrial which is pre-prepared by ovarian hormone stimulation (estrogens then progesterone).
Every step of this process is crucial and any disruption compromises the future pregnancy.
Infertility, a rising concern
We speak of infertility when a couple failed to achieve pregnancy after 1 year of regular contraception-free sexual activity. According to the Epidemiological Observatory of Fertility in France, this is the case of 18-24% of couples after one year of trial. After two years, couples who are still waiting to get pregnant are 8-11% (1). This number is gradually increasing.
Increasing older reproductive age
In France, couples decide more and more to have a child at an older age. The mean age of the first pregnancy increased from 25.1 years old between 1980 and 1984 (2) to 30 years old in 2011 (3). However, this increase in age is detrimental to fertility. After 38 years old, the egg cells stock begins to run out and egg cells have a less good quality.
Decline in the quality of sperm
A constant decline in the quality of sperm is also observed (number and/or mobility of sperm cells). The quantity of sperm cells decreases from 443.2 to 300.2 millions in 34 years (between 1976 and 2009). Actually, numerous factors have been implicated, notably environmental pollutants such as heavy metals and some organic pollutants (PCB…).
From now on, contrary to conventional wisdom; infertility involves men as often as women.
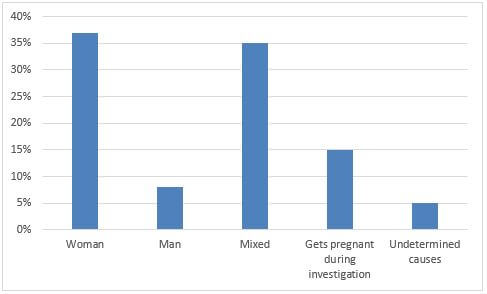
Origins of infertility – WHO study (4)
In 5% of cases, this infertility remains unexplained, no causes haven been found (4).
REFERENCES:
1 – BEH, INVS, N°7-8-9 du 21 février 2012 FERTILITÉ et Environnement : La perpétuation de l’espèce est-elle menacée?
2 – Maire Ni Bhrolchain M N et Beaujouan E, Bulletin mensuel d’information de l’institut national d’études démographiques : En France comme en Grande-Bretagne, l’allongement des études retarde les maternités, décembre 2012, numéro 495
3 – INSEE data, birth and fertility rates, TEF, 2012 edition
4 – Recent advances in medically assisted conception; WHO technical report series: Geneva 1992
Causes of infertility
There are many causes, sometimes hard to detect and often requiring thorough additional tests during diagnosis.
In women
Ovulation disorders are the main cause of infertility: Ovulation may be irregular (dysovulation) or totally absent (anovulation). Some of these anovulations are related to a polycystic ovary syndrome.
Distribution of the main causes of female infertility (1)
We also find:
- Fallopian tube damage: Blockage or damage, secondary to an infection (salpingitis), a congenital anomaly…
- Endometriosis: Pathological presence of endometrial glands outside of the uterus (in the ovaries, tubes, peritoneal cavity…)
- Infertility related to abnormalities of the cervix and its secretion
- Hormonal disorders, such as thyroid disorders, or uterine anomaly or pelvic abnormality, fibroma, polyps…
In men
Here again, there are many causes:
- Changes in the number, mobility and/or morphology of sperm cells
- Hormonal disorders such as male hormone deficiency
- History of trauma, surgery or infections
- Retrograde ejaculation, varicocele (dilated veins within the testicles)
- Genetic disorders, birth defects…
Between couples
Some behaviours or lifestyles are also harmful to the occurrence of a pregnancy: Tobacco, excessive alcohol, overweight, few or outside fertile period sexual intercourse, or even simply and unfortunately, being afraid …. of not having a baby!
REFERENCE:
1 – Recent advances in medically assisted conception ; WHO technicals report series: Geneva 1992
Management: first steps
Infertility evaluation
Medical tests are usually prescribed after a period of 18-24 months of unsuccessful sexual activity for a young couple without any known risk. For older couples, or couples with a history of eventual insufficient fertility, it is recommended to do the tests starting from the 6th month. It specifies the cause or causes of infertility relying, if needed, on additional tests that involve both partners (spermanalysis for men and hormonal examination for women). The outcome of these tests allows drawing a number of therapeutic solutions for the couple. Most of them are medical or surgical. If a major infertility is detected, the couple is referred straightaway to a center for assisted reproduction.
Initial medical treatments
The most frequent treatment of infertility is ovarian stimulation. It consists in stimulating the ovary with hormonal treatments (anti-estrogens or hormones such as FSH, usually secreted to stimulate the ovaries). We therefore obtain a simultaneous development of many follicles, each containing one egg. When the development is deemed satisfactory, ovulation is triggered by an injection. Other treatments (anti-infectives, etc.) are also prescribed according to an individual assessment, sometimes with vitamin supplementation (vitamin B12 and folic acid), notably in women with polycystic ovaries.
Reproduction surgery
In women, it is first of all a surgery of fallopian tubes. We can also remove endometrial lesions, pelvic adherences, polyps… in men, surgery mainly applies in case of atrophy of vas deferens or some important varicocele.
REFERENCES
1 – www.procreation-medicale.fr/infertilite/les-causesde-infertilite/
Assisted reproduction
Assisted reproduction or medically assisted procreation (MAP) consists in reproducing part of the natural process of fertilization, in a laboratory. Several techniques exist, each with precise indications. They allow considering serenely having children even in case of infertility.
Artificial insemination
It consists in collecting and preparing the spouse’s sperm to inject it in the woman’s uterus at the time of ovulation, most often after ovarian stimulation. Fertilization then occurs naturally, inside the woman’s body.
In vitro fertilization (IVF)
Eggs are obtained after important ovarian stimulation (FSH). Eggs are harvested then placed in culture, in contact with the spouse’s sperm cells harvested the same day.
1- Ovarian stimulation and ovarian puncture for oocyte retrieval
2- Putting sperm cells with oocyte for fertilization
3- In vitro development of the embryo
4- Embryo(s) transfer into the uterus
Embryos will then develop for 48 hours or even 5 days (what is called extended culture). They are then transferred into the womb for implantation.
Sperm microinjection
It involves the direct injection of sperm into an egg, instead of waiting for spontaneous fertilization to occur, just like in IVF. The other steps are identical to those of an IVF, from ovarian stimulation until embryo transfer.
Lastly, anonymous donations of embryos or gamete (oocyte and/or sperm) may be a last resort.
Nearly 3% of children are born today this way by MAP in France in 2012 (1).
REFERENCES
1 – Agence de biomédecine, Activité d’assistance médicale à la procréation 2012
Faq
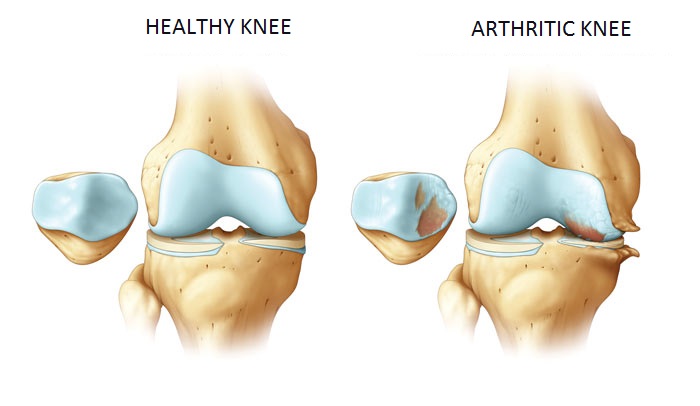
WHAT IS OSTEOARTHRITIS?
Osteoarthritis is a degenerative chronic condition, a form of rheumatism that progressively destroys the cartilage that covers the bones of some joints. It leads to a handicap with difficulties to move.
Osteoarthritis
Pain usually reveals osteoarthritis, otherwise, it goes unnoticed.
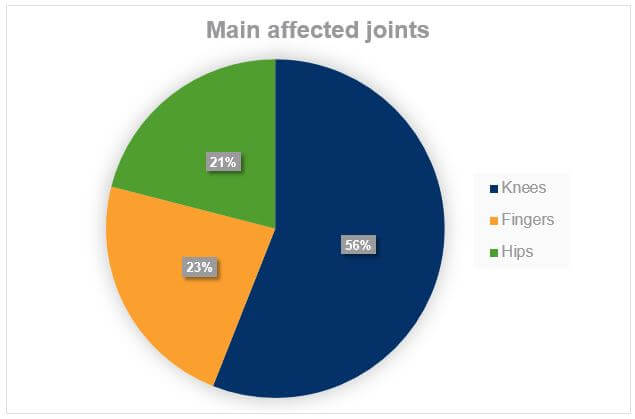
Main locations
Osteoarthritis mainly affects the joints of the knees, fingers, hips and cervical lumbar spine (1).
It may also affect the spine (cervical, lumbar vertebrae…), ankle, shoulders…
In general, several joints may be affected. We generally use the term generalized osteoarthritis when more than 3 joints are affected.
REFERENCES
1 – Richette. Généralités sur l’arthrose : épidémiologie et facteurs de risque. In Elsevier Masson, 2008.
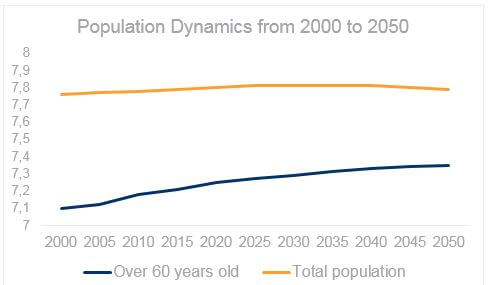
Osteoarthritis is the most common joint disease
Today, osteoarthritis affects nearly 10 million people in France: one French out of 6. It is one of the primary causes of invalidity in developed countries (1) and its frequency increases with age, despite the existence of juvenile forms. With the increase of elderly population and the expected doubling of the number of new cases by 2030; osteoarthritis is considered a true public health challenge.
Beyond the pain, this benign disease causes the loss of freedom of movement in time limiting progressively the mobility of affected joints. In 2005, osteoarthritis represents the second cause of invalidity in France, after cardiovascular diseases (2).
REFERENCES
1 – Brooks PM. Impact of osteoarthritis on individuals and society : how much disability ? Socials consequences and health economic implication. Curr. Opin. Rheumatol. 2002; 14 : 573-7
2 – Etude COART : Revue du rhumatisme 72 (2005) 1326-1330
Clinical symptoms of osteoarthritis
Pain is generally a revealing sign of osteoarthritis; being its main symptom. At the start of the disease, the pain is mechanical and marked by effort: It appears and deteriorates with the mobilisation of the affected joint and eases when rested.
In some people, a more or less long phase of stabilization may appear. However, osteoarthritis inevitably progresses.
The progression of osteoarthritis may also be associated with inflammatory outbreaks characterized by even painful swelling for a few days. In this case, pain persists at rest and may cause nocturnal awakening.
How is osteoarthritis diagnosed?
The treating physician will first ask about specifics on the pain characteristics, sensation of stiffness, and disruption of everyday life…. He/She will search for the presence of a reduced joint mobility, deformations, swelling.
He/She will rely on lab analyses and x-rays for more specifics, if necessary (presence of bone excrescence, narrowing of the joint space…)
He/She may ask for a rheumatologist or an orthopaedic surgeon opinion at an advanced stage.
Risk factors
Age is the first enabling factor but it is not the only one. Other factors are now well identified:
- Gender: Osteoarthritis is more frequent in women than in men and its frequency dramatically increases after menopause, especially osteoarthritis of the knees and fingers. Thus, osteoarthritis at the base of the thumb (carpometacarpal osteoarthritis) mainly affects women (80-90% of cases) and increases from 8% of women before menopause to 25% after.
- Genetics: Osteoarthritis runs in many families due to its inheritance nature (1).
- Traumas or repetitive strains: In case of high level sport activities or jobs exposed to repetitive violent movements or vibrations (pneumatic drills for miners, drillers…)
- Overweight: Overweight is responsible for overload on the knee joints (gonarthrosis). In women, obesity may multiply the risk of gonarthrosis by 9 especially through hormonal factors.
- Certain anatomic abnormalities: By modifying the normal weight borne by joints; some cartilage areas are overburden.
Osteoarthritis is therefore multifactor disease. Causes are complex and some of them, still little known, are still under investigation: Diabetes, hypercholesterolemia, hypertension…
REFERENCES
1 – Richette, Généralités sur l’arthrose : épidémiologie et facteurs de risques. In Elsevier Masson, 2008.
Treatments
Management of osteoarthritis targets on one hand pain relief, the most afflictive symptom, and on the other hand it limits its progression and the subsequent disablement that it creates. For this reason, experts recommend the combination of medical and non medical treatments and to individualize the treatment to each patient (1).
Thus, in case of pain, we usually prescribe analgesics or anti-inflammatory medicines (paracetamol or oral anti-inflammatory drugs for a short treatment period to limit digestive adverse events that are sometimes serious). These treatments are nowadays combined with more specific medicines for osteoarthritis called “anti-arthritics”.
Lifestyle is also a core part of the treatment and complement medicine-based treatments. Lifestyle maintenance is recommended by doctors in accordance to each patient way of life and needs: Possible reduction of overweight, regular physical activities during off periods of inflammatory outbreaks, physiotherapy, use of orthesis, use of canes…
The earlier this management occurs; the better controlled the progression of osteoarthritis. Therefore, it is better to consult your doctor upon the first signs as he/she will be the best to develop a global strategy.
REFERENCES
1 – Zhang W. et al., OARSI recommandations for the management of hip and knee osteoarthritis, Part II : OARSI evidence-based, expert consensus guidelines. Ostéoarthrisis and cartilage, 2008, 16, 137 – 162.
Fiche Arthrose de l’épaule
Fiche Arthrose digitale
Fiche Arthrose du genou
Fiche Ceintures lombaires
Fiche Eviter les effets indésirables des médicaments
Faq
WHAT IS SKIN?
Skin is the largest organ of our body. Its thickness varies depending on the different areas in the body from some tenth of millimetres in the eyelids to near 6 mm in the back.
The main role of the skin is to protect our organism from external aggressions, acting as a barrier. It also plays a major role on other vital functions, such as perception (touch), immunity, body temperature preservation as well as vitamin D synthesis.
The skin of our face is very sensitive and exposed to external aggressions. Daily care is essential and contributes to maintain appearance and health.
Healing
How does the skin heal?
Like all organs, the skin is equipped with repair and renewal capacities that help it heal: more or less rapidly and not always true. It all depends on the extent and depth of the injury.
The skin has three superposed layers: The epidermis at the surface, below there is the dermis which is rich in nourishing blood vessels and nerves, all located within a collagen and hyaluronic acid structure. Finally, in depth, there is the hypodermis.
If the injury is superficial and does not affect the epidermis, then the skin is able to renew itself provided causes of irritation are eliminated.
When the injury is more important, deep structures of the skin may be affected and the body unleashes a different cascade of reactions:
- Blood coagulates to stop bleeding, a blood clot forms.
- Defence cells called macrophages absorb eventually present debris and microorganisms to clean the injury: It is called the cleansing phase. During this phase that may last from a few hours to 4 days, the wound exudes colourless to slightly yellow liquid, called lymph, containing cleansing and stimulating substances that favour the emergence of vessels. The healing process has begun.
- To make up for the wound-induced loss of substance, the proliferation phase sets in. A new support tissue is constituted with collagen and hyaluronic acid synthesis by cells from the dermis. New vessels are created. This tissue proliferates to the surface of the skin.
- When this tissue sufficiently fills in the wound, the epithelium of the adjacent intact skin colonizes the surface of the wound. At the end of ten days, the crust falls to reveal a scar.
This natural healing process may be compromised by different factors, either the presence of foreign bodies, important hematoma, infection, and underlying disease but also by inadequate care.
Daily life wounds
Cuts, scratches, abrasions by a rough surface…small wounds of everyday life may seem harmless but they must be adequately treated to heal well, without any risk of infection.
First acts
- Compress the wound until the bleeding stops.
- Use physiological serum to clean; or in case of heavy contamination, you may first wash the affected area with soap and water (1). If too painful, do not insist.
- Protect the infection using an antiseptic, preferably colourless, to mask the progression of the wound. Avoid using alcohol.
- if needed, apply a bandage: Sterile gauze, sterile compress or pre-cut bandage.
In addition to classic bandages, there are more specific bandages (watertight, humid, hydrocolloidal…) as well as creams and healing compresses. Ask your pharmacist for advice.
Whatever the type of the wound, one must always check if anti-tetanus immunization is up to date.
When to consult?
- In case of any doubt for children and elderly and systematically for newborns.
- In case of extended wound, more than half the surface of the palm, or if very contaminated by foreign bodies.
- When the wound is located on the back of the hand, on the neck or near a natural orifice such as the eyes which are risky areas.
- In case of a disease that further weakens the victim: diabetes, corticoids treatment or anti-coagulants…
- In case of signs of infection: swelling, oozing, purulent drainage.
- If bitten by an animal or crush injury.
REFERENCES
1 – Prise en charge des plaies aux urgences SFMU 2005
Les brûlures
In everyday life, there are plenty of opportunities to get burned. Burns may be due to heat (90% of burns) and also to sunlight (sunburns) and rarely to electric current or a chemical product.
Mains causes of burns (1)
While little burns can be easily healed, more extensive or deep burns require immediate consultation.
Different types of burns
To assess their seriousness, burns are classified depending on their extent and depth:
- First degree burns: Only epidermis is affected. The skin is red, painful, even swollen. It’s the standard “sunburn” or a kitchen burn.
- Second degree burns: Dermis is affected. Very painful, the skin is pinkish and humid, blisters appear.
- Third degree burns: The affected area is deeper. The skin is usually white but may be brown or even black. Ironically, there is little or no pain because the nerve ends have been destroyed.
What to do?
When the burn is superficial, the extent is less than half the palm of the victim’s hand and is not located near a natural orifice, topical care is sufficient.
First degree burn
- Cool down the burn by splashing fresh water for at least 5 minutes. This limits the progression of lesions;
- Apply an antibacterial-free hydrating cream or ointment (2). There are burn specific creams and ointments. Ask your pharmacist for advice.
Little extended second degree burn
- Do not cut through the blisters as they protect from infections and reduce the pain;
- Wash with fresh water;
- Disinfect the wound with an alcohol-free antiseptic as there is a risk of infection if blisters are cut;
- Protect the wound using specific bandages “non adhereing wound dressing” type, “membrane dressing” type or with antibacterial ointments or bandages (2).
Consult your doctor in case of any doubt or in case of more extensive burn. In case of serious burn, call SAMU/Center 15.
REFERENCES
1 – Carsin H. Prise en charge des brûlures en milieu non-spécialisé. Médecine d’urgence 2003.
2 – Recommandations S.F.E.T.B- Brûlures, mars 2006, vol VI, n°4, p215-217.
Leg ulcers
Poor blood circulation, either due to venous insufficiency or atherosclerosis, leads to complications including leg ulcer. It is defined as a wound, a loss of substance affecting the skin up to the dermis, particularly difficult to heal with a risk of infection.
Signs
Ulcers of venous origin, by far the most common (80% of leg ulcers), represent a very progressive stage of chronic venous insufficiency (varicose vein, or more frequently, history of thrombosis). It appears progressively, most often within the ankles, and is generally not painful. Which is the entire issue! In absence of treatment, the ulcer becomes chronic. One should always check any wound in the leg.
Arterial ulcer is less frequent and rather affects men aged over 50 years old with vascular risk factors (tobacco, hypertension, obesity…). Unlike the previous, it appears brutal, mostly after a shock, and is very painful.
In both cases, immediate consultation is advised.
Medical care
To heal a leg ulcer, it is not enough to just treat the wound, one must also treat the cause.
The wound will be cleaned; residues that are hindering the healing process will be removed. Conducive local conditions will then be restored using bandages that adapt to each healing phase. After the detersion phase, interface, hydrocellular, hydrocolloidal, Vaseline or hyaluronic acid containing dressings will be used.
In parallel, what caused the ulcer will be treated. If it is of venous origin, a venous contention will be positioned using specific dressing. In case of arterial ulcer, the patient will be advised to limit the cardiovascular risk factors (tobacco, arterial hypertension, overweight…).
REFERENCES
1- Recommandations HAS, 2011
Wounds and diabetes
People with diabetes know the attention they should pay, particularly, to their feet. Because a poorly controlled diabetes exposes the patient to healing difficulties in case of injury, even in case of a wound that went undetected for a very long time. Eventually, there is a risk of amputation.
Globally, 15% of diabetic patients will present a foot ulcer at one moment of their lives (1). An old or a poorly controlled diabetes may, in fact, cause a loss of sensitivity within extremities which favour the occurrence of injuries as well as vascular disorders that are detrimental to healing, with an increased risk of infection due to the decrease in immune defences.
More worryingly, some wounds may pass completely undetected. It’s the case of the “diabetic foot ulcer”, ulceration at the sole of the foot which is luckily increasingly rare, is deep and painless and may progress undetected. This is why it is advised to daily inspect the feet of a diabetic person with regular visits to the chiropodist (1). Consultation is required even with the smallest injury!
Medical care
Within the wound, the best possible conditions are to be established to help the healing process. This is achieved by dehorning (horn removal) and debridement around the wound using a lancet, then application of a bandage specific to each healing phase. After the detersion phase, interface, hydrocellular, hydrocolloidal, vaseline or hyaluronic acid containing dressings will be used to significantly reduce the size of the ulcer.
On a general level, controlling diabetes is imperative to heal. In case of diabetic foot ulcer, the foot will be strictly and permanently offloaded until healing, ideally with suitable shoes.
REFERENCES
1 – HAS 2011, Les pansements indications et utilisations recommandées
Cracks and infant diaper rashes…
Cracks
Cracks are skin injuries that are due to severe drought and repetitive aggressions by the cold, irritant products (detergents), intensive pressures (foot cracks) or repetitive micro-trauma (cracked nipples when breastfeeding). Usually shallow, they must be treated in time to avoid exacerbation and pain.
The solution: Regularly hydrate the skin.
There are a number of hydrating creams. Some are specifically formulated without aggressive components (perfume, conservatives…) to respect fragile skin. They hydrate, relieve and favour skin repair.
Infant diaper rash
Diaper rash is an irritation that alters the superficial layer of the skin. It is localized in the areas that are covered by diapers (bottom, genitalia, and inner thighs) and is displayed by a dry or exuding redness, with or without small spots. In most cases, it is due to the rubbing of diapers against the skin, diapers that are too tight or not enough changed. Contact with urine and faeces also cause a chemical “burn” that is increased if the baby suffers from diarrhoea. The natural protection that is ensured by the skin is disrupted and must be re-established as soon as possible to limit the risks of infection.
What to do?
Avoid all sources of maceration of the skin by leaving the baby diaper free whenever possible. Apply a soothing and protecting cream after every nappy change: Zinc oxide, copper sulphate, dexpanthenol based creams or healing care products that are conceived to repair as soon as possible the weakened skin of the baby. Ask your pharmacist for advice.
Faq
Dermatosis (dermatitis, psoriasis, vitiligo)
Dermatitis
Dermatitis is characterized by intense itching and is one of the most frequent skin diseases responsible for nearly 30% of consults in dermatology. It’s a chronic inflammatory disease of multiple origins including allergy being the main cause. It is characterized by the presence of poorly defined red plaques, sometimes associated with small transparent blisters that may converge in bubble, break, and seep then form a crust.
There are two major types of dermatitis.
Contact dermatitis
It is only observed when there is contact with substances –so called allergenic – i.e. causing an allergic reaction. These substances may vary from one person to another: medicines, hair dyes, plastic (latex gloves), metals (earrings)…the doctor will use skin tests to identify which substance causes the allergy.
Atopic dermatitis
Atopic dermatitis is determined by a hereditary predisposition to develop allergic reactions associated with a genetic abnormality which renders the skin “permeable” to some substances. This is the case of some food among infants and substances in the air among older (pollen, dust mite…).
Main localizations of dermatitis:
- cheeks
- elbows
- forehead
- knees
Atopic dermatitis progresses naturally with age:
- In infants, flare-ups are frequent and are essentially present in the cheeks and forehead;
- After the age of 2, the dermatitis become more chronic, it rather affects the skin folds (elbows, knees); as a result of scratching, the skin becomes dry and thick.
- Dermatitis declines in 85-90% of cases in adolescents and adults.
Psoriasis
Psoriasis is a skin disease characterized by red plaques covered by dead skin, dandruff that gets loose easily. Psoriasis is neither infectious nor contagious; in most cases, it is benign but may prove to be particularly inconveniencing in case of visible lesions. Psoriasis is relatively frequent affecting nearly 2% of the population (1,2). It affects both children and adults with two peaks of frequency: around twenty (young adult) and around fifty.
Specific localizations
It is a chronic disease that progresses with inflammatory flare-ups. There are many types of psoriasis. The most common is plaque psoriasis. Plaques are little widespread; well defined with some itching. They are most often localized symmetrically within areas that are exposed to contact (elbows, knees, anterior surface of tibias, sometimes in the scalp and lower back).
Main localizations of dermatitis:
- elbows
- knees
- tibias
Other types are rarer, such as the guttate psoriasis, with drop-like lesions separated and dispatched all over the body. In a certain number of cases (2), psoriasis may be complicated with the occurrence of a joint damage called psoriatic arthrisis.
Very fast cellular renewal of the epidermis
Psoriasis is caused by a cellular renewal of the superficial layer of the skin that occurs too fast, thus building up and forming plaques. Two factors come into play in the occurrence of flare-ups: a hereditary predisposition combined with triggering factors such as an infectious disease, intake of some medicines, stress or even repetitive trauma on the skin (rubbing of clothes)…
Psoriasis is an unpredictable progressive chronic disease that requires medical attention.
REFERENCES
1 – CEDEF, Item 123-Psoriasis, Ann Dermatol Venereol 2012; 139, A112-A120
2- Clabaut A. et al., Prise en charge du Psoriasis chez l’enfant, Ann Dermatol Venereol 2010; 137, 408-415
Treatment of dermatitis and psoriasis
Presently, dermatitis and psoriasis, which are both chronic inflammatory disorders, can be considerably soothed. A wide range of treatments may in fact soothe the symptoms and reduce the visibility of lesions, thus improving the quality of life.
For these skin disorders, precedence is given to local treatments. They are based on local application of corticoids, called dermocorticoids (1,2). Their effect is usually spectacular on both lesions and itchings. They exist in different forms, prescribed depending on the nature and localization of plaques: ointment, cream, gel, lotion or even medicated plasters. Other treatments may be associated to reduce the thickness of plaques or heal a possible secondary infection… in case of intensive itching, oral antihistamines are prescribed. More intensive treatments, such as immunosuppressant, are reserved for serious disorders.
Phototherapy using UV light may also be useful for certain people. It is prescription-only and practiced only by a dermatologist.
How to protect the skin on a daily basis?
These disorders are characterized by a skin that is too dry and uncomfortable, with pulling. Protecting the skin is an essential part of the treatment:
- Hydrating the skin with bath oils, lipid-enriched soaps and emollient creams. Avoid the use of classical soaps.
- Do not scratch the lesions. In case of itching, simply press on the “scratchy” area.
- Avoid too tight clothing, synthetic materials and wool. Favour cotton and linen.
- Use soft detergents when washing clothes.
REFERENCES
1 – CEDEF, Item 123-Psoriasis, Ann Dermatol Venereol 2012; 139, A112-A120
2- Darsow U. et al., EFTAD/EADV eczema task force 2009 position paper on diagnosis and treatment of atopic dermatitis. J Eur Acad Dermatol Venereol 2010; 24 ; 317-28
Vitiligo
White spots, smooth, sometimes with a certain relief… these are the characteristics of vitiligo, a chronic skin disorder, benign, painless and non contagious but often hard to live with because of an esthetical prejudice.
Characteristic white spots
Vitiligo appears in 50% of cases between 10 and 20 years old (1), but mainly between the age of 20 and 30. Depigmented white spots or plaques appear anywhere on the body but there are preferred areas: Back of the hands, feet, elbows and knees, areas located in the folds of the skin… the number of spots is variable, two to three small spots or wide plaques on the entire body. The progression is unpredictable; vitiligo may widen or rarely, repigment itself spontaneously, especially in sun-exposed areas.
A melanocyte failure
Vitiligo is due to a local loss of melanocytes*, cells that colour and pigment the skin. Precise cause of their loss remains unknown until today. Inheritance definitely plays a role: In nearly 30% of cases, there is a family history. Immune disorders are also responsible: called an auto-immune disorder, which means a disease in which the immune system, usually destined to fight micro-organisms from the outside, will make a mistake on the enemy and destroys wrongly the melanocytes of the skin (1).
The specific cause of vitiligo is therefore unknown, but there are triggering factors that favour the occurrence of plaques: overexposure to the sun, stress, local micro-trauma within rubbing areas of the skin, such as hands, elbows and knees.
*melanocytes are cells that pigment the skin
REFERENCES
1 – www.orpha.net/data/patho/Pub/fr/Vitiligo-FRfrPub672v01.pdf – Décembre 2006
Treatment of vitiligo
Actual treatments help reduce the size and the number of spots or to repigment the skin by giving back a coloured appearance.
When spots are recent and remain localized, it is possible to stimulate the production of pigments by melanocytes that are still present using local corticoids called dermocorticoids. Best results are obtained on the skin and neck, with recent lesions and dark skins (1). These skin repigmentation solutions (dermocorticoids) may be associated with immunomodulators** that also contribute to skin repigmentation.
Phototherapy, using UV light, is practiced in children and people suffering from generalized vitiligo or people who are treatment resistant to previous therapies. More recent, laser targeted phototherapy appears efficient and well tolerated.
When the outcome is not possible with repigmentation treatments, one might consider a menalocyte transplantation. The transplantation allows implantation of melanocytes taken from the patient itself on the depigmented area. The last evolution of this technique consists in implanting melanocytes in suspension and provides efficient outcomes (2).
**medicine that stimulates or represses the immune system reactions
How to limit the spots?
While waiting for the outcomes of medical treatment, self-tanning creams or special colour correction may be used to camouflage patches.
Although the sun has renown skin pigmentation virtues, it may only be used in the controlled framework of a heliotherapy*** prescribed by a doctor. In other cases, it is essential to protect the very fragile pigmented areas: sunscreen and covering clothes are necessary even in winter or cloudy weather.
***medical treatment by exposure under solar radiation
REFERENCES
1 – Taieb A et al.Guidelines for the management of vitiligo: the European Dermatology Forum consensus. Brit J Dermatol 2013; 168:5-19.
2 – Mulekar SV, Al Issa A, Al Eisa A. Treatment of vitiligo on difficult-to-treat sites using autologous noncultured cellular grafting. Dermatologic surgery 2009;35(1):66-71.
Faq
Le vieillissement cutané
La peau et ses constituants
 Sensible, réactive, émotive quand elle rougit, la peau reflète nos émotions, notre vitalité et, avec le temps, notre âge.
Sensible, réactive, émotive quand elle rougit, la peau reflète nos émotions, notre vitalité et, avec le temps, notre âge.
Pour assurer ses multiples fonctions, en premier lieu nous protéger des coups, des blessures et des micro-organismes, notre peau est constituée de trois couches :
- L’épiderme, en surface : recouvert d’une couche cornée protectrice et truffé de terminaisons nerveuses sensorielles, il est imperméabilisé par le sébum, une substance grasse, et équipé de cellules productrices de mélanine, le pigment qui protège du soleil.
- Le derme, situé en dessous de l’épiderme : structure de soutien, il est doté d’une armature de fibres de collagène et d’élastine baignant dans un gel de protéoglycannes. Il contient toutes les structures nécessaires au fonctionnement de la peau : vaisseaux sanguins, follicules pileux, glandes sudorales ou sudoripares, glandes sébacées productrices de sébum et les cellules fibroblastes sécrétant l’armature fibreuse ainsi que l’acide hyaluronique.
- L’hypoderme, en profondeur: c’est un isolant thermique disposant de réserves énergétiques en graisses.
Les composants essentiels pour la tonicité de la peau
- Le collagène du derme : les fibres de collagène, reliées par des filaments d’élastine, constituent une véritable armature pour la peau et lui permet de résister aux coups et aux chocs.
- Il assure tonicité et résistance
- L’acide hyaluronique : inséré entre les fibres de collagène, il possède d’excellentes propriétés hydratantes en retenant jusqu’à 1000 fois son poids en eau et crée ainsi un « matelas » hydraté et rebondi.
- Il procure souplesse et hydratation
- Les anti-oxydants, présents dans toutes les cellules de la peau : ils maintiennent l’intégrité de la peau en neutralisant les radicaux libres. Les radicaux libres sont des composés toxiques issus du métabolisme des cellules et des agressions extérieures (soleil, infections, inflammations …). S’ils ne sont pas neutralisés, ils détruisent les structures alentour et l’on estime aujourd’hui qu’ils sont les principaux responsables du vieillissement.
Pour piéger ces radicaux libres, notre alimentation nous procure des antioxydants naturels. Ils constituent la principale défense contre le vieillissement
Au fil des années, la peau perd peu à peu sa tonicité et, dès l’âge de trente ans, les premières ridules apparaissent.
En surface, l’épiderme s’amincit, il n’arrive plus à se régénérer suffisamment vite. La sécrétion de sébum baisse et la peau devient plus sèche.
Le derme, lui aussi, diminue d’épaisseur. Ses cellules, qui ont pour rôle de sécréter et renouveler le collagène, l’élastine et l’acide hyaluronique, deviennent moins performantes. La synthèse et la qualité de ces composants essentiels diminuent, l’armature du derme se désorganise, le matelas d’acide hyaluronique se « dégonfle ». La peau perd ainsi progressivement sa tonicité, sa souplesse et ses volumes.
Puis les rides se creusent en profondeur, la peau se relâche, le contour du visage s’affaisse.
Ce processus de vieillissement naturel, contrôlé par des facteurs génétiques et hormonaux, est en grande partie inéluctable. A la ménopause par exemple, il s’accentue consécutivement à la baisse de la sécrétion d’oestrogènes.
Le vieillissement cutané peut cependant s’accélérer considérablement sous l’effet de facteurs extérieurs, environnementaux, contre lesquels, fort heureusement, on peut lutter !
Les agresseurs extérieurs
- le soleil : favorise la formation de nombreux radicaux libres qui agressent les cellules cutanées et provoquent leur mort prématurée.
- le tabac : rétrécit le diamètre des petits vaisseaux qui nourrissent la peau et l’alimentent en micro-nutriments, fragilisant ainsi les cellules cutanées.
- le stress : augmente la production de radicaux libres.
- la pollution atsmosphérique : diminue les défenses du système immunitaire.
- une alimentation déséquilibrée, pauvre en légumes et en fruits : si les apports en antioxydants sont insuffisants, les radicaux libres attaquent les membranes cellulaires, dégradent le collagène et l’acide hyaluronique.
Une certaine hygiène de vie permet donc d’atténuer sensiblement l’effet des facteurs nocifs de l’environnement, tout comme le permet l’usage quotidien de soins cosmétiques protecteurs.
Les soins au quotidien
 Indispensables au quotidien pour le maintien d’une peau en pleine santé, les soins cosmétiques contribuent à retarder l’apparition des signes du vieillissement, notamment en protégeant la peau des agressions externes, et à les atténuer.
Indispensables au quotidien pour le maintien d’une peau en pleine santé, les soins cosmétiques contribuent à retarder l’apparition des signes du vieillissement, notamment en protégeant la peau des agressions externes, et à les atténuer.
Si la plupart agissent sur les couches supérieures de l’épiderme, il existe des actifs agissant en profondeur, pour un lissage accru de la peau. Certains actifs sont capables de relancer la synthèse des composants majeurs de la peau et de favoriser le renouvellement des cellules fibroblastiques (acide hyaluronique, collagène…)(1). Ces actifs peuvent être associés à des ingrédients anti-oxydants protecteurs contre le vieillissement prématuré (coenzyme Q10, flavonoïdes anti-oxydants, extraits de plantes, vitamines C et E …).
Les compléments alimentaires
Ils permettent de renforcer l’effet anti-âge des soins dermo-cosmétiques, à condition d’offrir, là aussi, une composition adaptée aux besoins de la peau. Ils devront donc apporter à la fois des anti-oxydants et des composants nutritifs du derme ainsi que, idéalement, des principes actifs régénérants. L’effet des compléments alimentaires est optimal en utilisation quotidienne, en association avec des dermo-cosmétiques adaptés.
REFERENCES
1 – An JJ, Eum WS, Kwon HS, Koh JS, Lee SY, Baek JH, et al. Protective effects of skin permeable epidermal and fibroblast growth factor against ultraviolet-induced skin damage and human skin wrinkles. J Cosmet Dermatol 2013 Dec;12(4):287-95.)
Les traitements médicaux et chirurgicaux
La médecine esthétique
Elle s’adresse principalement aux rides profondes et tenaces. Différentes techniques de rajeunissement sans chirurgie sont disponibles, leurs indications sont à apprécier par le médecin.
- Peeling: exfoliation chimique des couches superficielles de la peau pour en améliorer l’aspect et gommer certains défauts.
- Dermabrasion: « ponçage » mécanique léger des couches superficielles de la peau.
- Photo-rajeunissement par lumière pulsée (stimulation de la production de collagène par la lumière) ou par laser (abrasion des couches superficielles de la peau).
- Injections: les injections de produits de comblement sont aujourd’hui en plein développement, à commencer par les injections d’acide hyaluronique, produit majeur des cabinets de médecine esthétique.
L’acide hyaluronique
Naturellement présent dans notre corps, en particulier dans le derme qui contient 50 % de l’acide hyaluronique de l’organisme, l’acide hyaluronique est utilisé depuis de nombreuses années par les médecins en injections au niveau des rides. Une fois injecté, il agit comme une éponge et se gorge d’eau, apportant volume, souplesse et gonflant aux tissus cutanés. L’acide hyaluronique permet ainsi de redessiner les contours du visage, de combler les creux disgracieux et de gommer, de l’intérieur, les rides même profondes.
De la même façon, il permet d’atténuer les cernes sous les yeux.
Le Botox®
La toxine botulique permet d’immobiliser temporairement les muscles, elle est utilisée en injections intramusculaires pour limiter les rides d’expression.
La chirurgie esthétique
Lorsque les soins et la médecine esthétique ne suffisent plus à masquer les rides et l’affaissement du visage, la chirurgie esthétique, réalisée sous anesthésie locale ou générale, peut être indiquée après consultation d’un chirurgien plastique qualifié.
- Lifting : On pratique des incisions pour décoller et retendre la peau.
- Remaillage: Des fils d’or sont insérés sous la peau afin de la retendre.
- Lipofilling : On injecte au niveau des rides de la graisse prélevée sur les cuisses, les hanches ou le ventre du patient.
Les bénéfices de la médecine et de la chirurgie esthétique devront être entretenus au quotidien par des soins cosmétiques adaptés.
Faq
Contactez-nous
Dernière mise à jour le : 23/07/2015